Questions Surrounding Palliative Care; Simplified
What is Palliative Care?
The World Health Organization defines palliative care as an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering using early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial, and spiritual.”
What is at the core of Palliative care?
The core of palliative care is addressing, in-depth, the physical, emotional, and spiritual suffering that a patient may experience. Palliative care is a crucial component in oncologic care, and integrating it into the care plan for patients with advanced cancer is highly recommended. Early integration of palliative care has proved to provide improved outcomes in patients with advanced cancer.
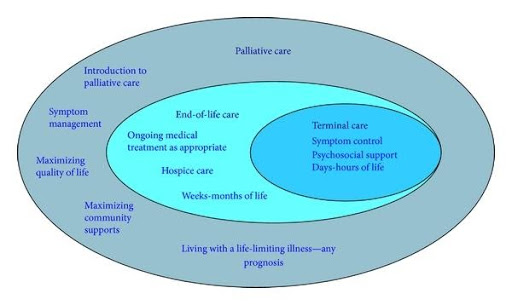
What is the difference between Palliative Care and Hospice?
Palliative care is whole-person care that seeks to relieve symptoms of various diseases at any stage. It is applicable for any trajectory of the disease.
Hospice focuses on end-of-life; care for patients who likely have six months or less to live.
Essentially hospice care is always palliative, but not all palliative care is hospice care.
Yet where you are in the course of your illness makes all the difference in whether you are eligible for hospice or palliative care. To qualify for hospice, a doctor must certify that death could be expected in six months or less if the illness runs its natural course. The individual must also not be receiving curative treatment, such as chemotherapy. On the other hand, patients can use palliative care anytime during a severe illness—starting with the diagnosis—and patients can be receiving curative treatments for their disease.
Who should receive palliative care and why?
Any person diagnosed with a chronic, severe illness or complex medical issues. The understanding that these serious illnesses often lead to physical, emotional, spiritual, and social issues. Examples of appropriate illnesses include cancer, hematologic malignancies, end-stage chronic obstructive pulmonary disease (COPD), end-stage congestive heart failure, end-stage kidney disease, end-stage liver disease, dementia, stroke, and many others.
Palliative care can be helpful at any stage of illness and is best when provided from the point of diagnosis. Also, necessary when patients first begin treatment with chemotherapy. Although symptoms may not be present initially, we can serve as a resource should unwelcome side effects develop.
Why is palliative care important in cancer care?
For our patients, it is essential to remember that the effects of cancer and its treatments vary from person to person. Our palliative care team works to assess each patient’s situation and works together to develop the best care plan for the patient and their family. The focus is on having a better quality of life, less pain, less shortness of breath, less depression, and less nausea. Research has also shown that cancer patients receiving palliative care have better emotional health because their medical care aligns with their values, goals, and preferences. It is essential to improve patients’ quality of life by approaching care from a more holistic approach. It looks at the patient as a whole person; it does not only look at the disease.
How can palliative care help?
- Palliative care can control physical symptoms and side effects such as pain, shortness of breath, fatigue, anxiety, depression, sleep issues, lack of appetite, nausea, constipation, or diarrhea.
- It can manage emotional issues that go alongside cancer diagnosis and treatment.
- Assessing spiritual concerns
- Supporting the needs of caregivers
- Addressing concerns regarding advanced care planning. Assisting with an explanation of documents and filling out advanced care planning forms, ie, MOLST forms
- Transitioning to hospice care services if and when applicable
- Your palliative care team will ask what is most important to you. Maybe you would like to feel well enough to leave the hospital or move forward in your treatment. Perhaps you wish not to be hospitalized at all. Or you may have a special event that you want to be strong enough to attend. Your oncology and palliative care team together can help you try to reach those goals.
If I agree to palliative care, does that mean I am giving up?
Not at all! The goal of palliative care is to help you achieve the best possible quality of life while undergoing treatments or living with a chronic illness. PC seeks to alleviate or help you cope with symptoms you experience while undergoing aggressive treatments that aim to cure or stabilize your illness. By getting pain and distressing symptoms under control, you can focus on fighting the disease.
Who can be part of the palliative care team?
The team comprises palliative care specialist doctors, advanced practice nurses, nurses and includes social workers, nutritionists, and chaplains. Its focus is not to treat or cure your disease but to ease your symptoms and any side effects of treatment. If anyone has questions regarding palliative care services or feels someone may be eligible and unsure, please just reach out. Any of the providers would be willing to answer questions or discuss options. Also, it is important to remember that referrals can come from anyone who feels that a patient is eligible.